Last week we explored the impact laparoscopy has on the pulmonary and cardiovascular systems.
So how can we manage our patients’ anaesthetic to achieve the best possible outcome when performing laparoscopic procedures?
Ventilatory support in the form of intermittent positive pressure ventilation (IPPV), with a mechanical ventilator, is recommended for patients where the procedure is anticipated to last longer than 15 minutes.
Mechanical ventilation should be commenced once the patient is stable under general anaesthesia as follows:
1. Monitor ETCO2 – the normal range is 35 mmHg – 45 mmHg and this is crucial for decision making about the ventilation requirements of the patient.
2. Tidal volume 10 – 20ml/kg – set the ventilator at 10 ml/kg and increase as required. In order to avoid barotrauma, it is wise to set tidal volume at no more than 20ml/kg, and to adjust the respiratory rate.
3. Respiratory rate 10 – 12 breaths/min, adjusted to the requirement of the patient. Changing the rate up or down based on the degree of increase or decrease, respectively, in ETCO2 is a sound strategy to manage ventilation. This protects the lung from being damaged by barotrauma due to over ventilation in the face of an expanded abdomen and minimises the decrease in venous return that occurs when the thorax is expanded due to positive pressure ventilation. Blood pressure monitoring is strongly recommended for laparoscopic procedures.
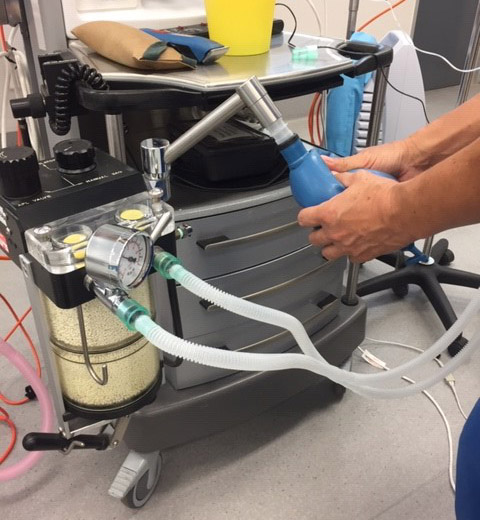
While mechanical ventilation is recommended, it is possible to manually or hand ventilate a patient during laparoscopy of longer than 15 minutes duration. If this is the only option available then a dedicated person, or “human ventilator”, is recommended to squeeze the reservoir bag to provide a breath to the patient, during the procedure.
Manual positive pressure ventilation criteria:
1. Monitor ETCO2 – essential to the success of any IPPV whether it is instituted mechanically or manually, because this guides you to successful beginning and end points of ventilation.
2. Use a manometer (pressure gauge) connected to the breathing system so that you know what pressure you are delivering, ideally 10 – 12 cm H20. If you don’t have a manometer then observe the thorax as you deliver a breath and make sure that this looks like a reasonable respiratory excursion. Remember positive pressure ventilation impacts the cardiovascular system by decreasing venous return, lowering cardiac output and blood pressure. Again, blood pressure monitoring is strongly recommended.
3. Respiratory rate see Point 3 above.
Laparoscopy is such a valuable skill to utilise in your clinic. Appropriate planning, and vigilant monitoring of ETCO2 and blood pressure during anaesthesia will help achieve an optimal outcome for your patients.
If you want to learn more about Laparoscopy this is the workshop you don’t want to miss! Dr Brenton Chambers, Dr Peter Delisser & Dr Kathryn Duncan are combining their expertise and we’re keen to share it with you. This workshop is proving to be very popular so don’t delay! Register HERE for the Laparoscopy: Principles and Practice Workshop at Gatton on February 7-9, 2020.
Other interesting reads:
Part 1: Anaesthetic considerations during Laparoscopy
From Laparoscopy to surgery on large land-based predators (Dr Brenton Chambers)
A peek into Laparoscopy with Dr Peter Delisser
Dr Kathryn Duncan joins the laparoscopy educator team
