With the recent increased popularity of brachycephalic dog breeds, and their all too common respiratory problems, it’s not surprising that VetPrac’s upcoming “Fix the Face” workshop filled up quickly. If you’re one of the lucky vets that managed to snare a spot for this year’s workshop, we thought we’d whet your appetite with a few case studies demonstrating the importance of thorough clinical and radiographic investigation prior to surgery, as well as always warning owners about the risk of recurrence of elongation of the soft palate post-resection surgery. Thanks to Dr. Charles Kuntz and Dr. Abbie Tipler for providing these case studies. Both Charles and Abbie are educators at the workshop this year; VetPrac looks forward to welcoming Charles and Abbie back to the education team; they always give 110 % at the workshop and we love having them both in our team.
If you missed out on this years’ workshop, register your interest in future Fix the Face workshops via this .
Case report by Dr Abbie Tipler: Brachycephalic Airway with a Co-Morbidity of Hiatus Hernia
Signalment: 2-year-old male French Bulldog, Charlie
History: 1-year history of daily regurgitation. This had resulted in several bouts of aspiration pneumonia; he had been treated with several courses of antibiotics which seemed to help temporarily. There was no history of airway signs, for example snoring, exercise intolerance, stertorous breathing, cyanotic or collapse episodes and the primary presenting sign was regurgitation with secondary aspiration pneumonia leading to coughing. His airway had been previously assessed as normal.
Physical examination and investigations: On upper airway examination, the soft palate was elongated, the laryngeal saccules were oedematous, and the nares were stenotic.
The workup for Charlie included routine bloods, chest radiographs and upper GI endoscopy.
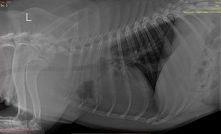
Chest radiographs revealed signs of aspiration pneumonia.

Upper GI endoscopy revealed fluid pooling in the caudal oesophagus, dilation of the gastro-oesophageal sphincter, oesophagitis, and a mild hiatal hernia.

Diagnosis: Aspiration pneumonia secondary to regurgitation with background of hiatus hernia, and elongated soft palate, oedematous laryngeal saccules and stenotic nares.
Decision making: The decision to be made was whether to treat just the airways in the hope that the hiatal hernia would settle with reduced upper airway pressure, or to concurrently repair the hiatal hernia. There is some controversy amongst specialists in the approach to take here.
In this case, given the ongoing aspiration pneumonia, we wanted to give the best chance of a resolution of the regurgitation. There is also current research around the anatomy of the oesophageal hiatus, in French Bulldogs particularly, and it appears that they are particularly prone to anatomical laxity of this region (increasing the risk of upper GI signs).

Treatment: Charlie was treated with a further one week of broad-spectrum antibiotics and omeprazole to help treat the aspiration pneumonia and regurgitation prior to surgery, however, given the chronicity of the changes in the lungs and the ongoing regurgitation, it was not expected we could completely resolve this prior to surgery.
Charlie was anaesthetised and we repaired (firstly) the hiatal hernia with a herniorrhaphy, oesophagopexy and gastropexy, and then corrected the airways with a staphylectomy, sacculectomy and nares wedge alarplasty. In general instances, we avoid performing concurrent procedures with airway surgery, however, if we do, we perform the concurrent procedure first. The reason for avoiding concurrent procedures is that we try to reduce the time under anaesthetic so there is the least possible compromise to the lungs during recovery from anaesthesia, which is a risk period. In this instance, however, the regurgitation/aspiration was also a risk to the overall airway recovery. The patient’s recovery was uneventful. All post-operative precautions were taken including careful one-on-one monitoring, micro-dose medetomidine on recovery if stressed/panting, oxygenation as required.
Discharge medications: 6-week course of amoxicillin-clavulanic acid antibiotic at 20mg/kg for the aspiration pneumonia, and 6 weeks of BID omeprazole 1mg/kg.
Recheck at 6 weeks: the aspiration pneumonia had cleared; the patient was no longer regurgitating.
Take-home messages for this case:
Always consider plain film radiographs of the chest prior to airway surgery.
Consider further diagnostics e.g. upper GI endoscopy if there are signs of regurgitation. Hiatal hernias are reasonably common in brachycephalic dogs, however, in many instances the GI signs will resolve when the airways are corrected.
Always examine the upper airway for yourself, as this was an example of where the upper airway had been previously noted to be normal.
Consider post-operative medical management of GI symptoms post airway surgery.
CLICK TO READ ANOTHER CASE STUDY BY DR. CHARLES KUNTZ
